Nicotine replacement therapy
A nicotine patch is applied to the left arm | |
| Clinical data | |
|---|---|
| Trade names | Nicoderm, Commit, Nicorette, others[1] |
| Other names | NRT |
| AHFS/Drugs.com | Template:Drugs.com |
| MedlinePlus | a601084 |
| Script error: No such module "Engvar". data | |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| Script error: No such module "collapsible list". | |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| E number | {{#property:P628}} |
| CompTox Dashboard (EPA) |
|
| ECHA InfoCard | {{#property:P2566}}Script error: No such module "EditAtWikidata". |
| Chemical and physical data | |
| Formula | |
Expression error: Unexpected < operator.Expression error: Unexpected < operator.Expression error: Unexpected < operator.
Nicotine replacement therapy (NRT) is a medically approved way to treat people with tobacco use disorder by taking nicotine through means other than tobacco.[6] It is used to help with quitting smoking or stopping chewing tobacco.[1][7] It increases the chance of quitting tobacco smoking by about 55%.[8] Often it is used along with other behavioral techniques.[1] NRT has also been used to treat ulcerative colitis.[1] Types of NRT include the adhesive patch, chewing gum, lozenges, nose spray, and inhaler.[1] The use of multiple types of NRT at a time may increase effectiveness.[9][10]
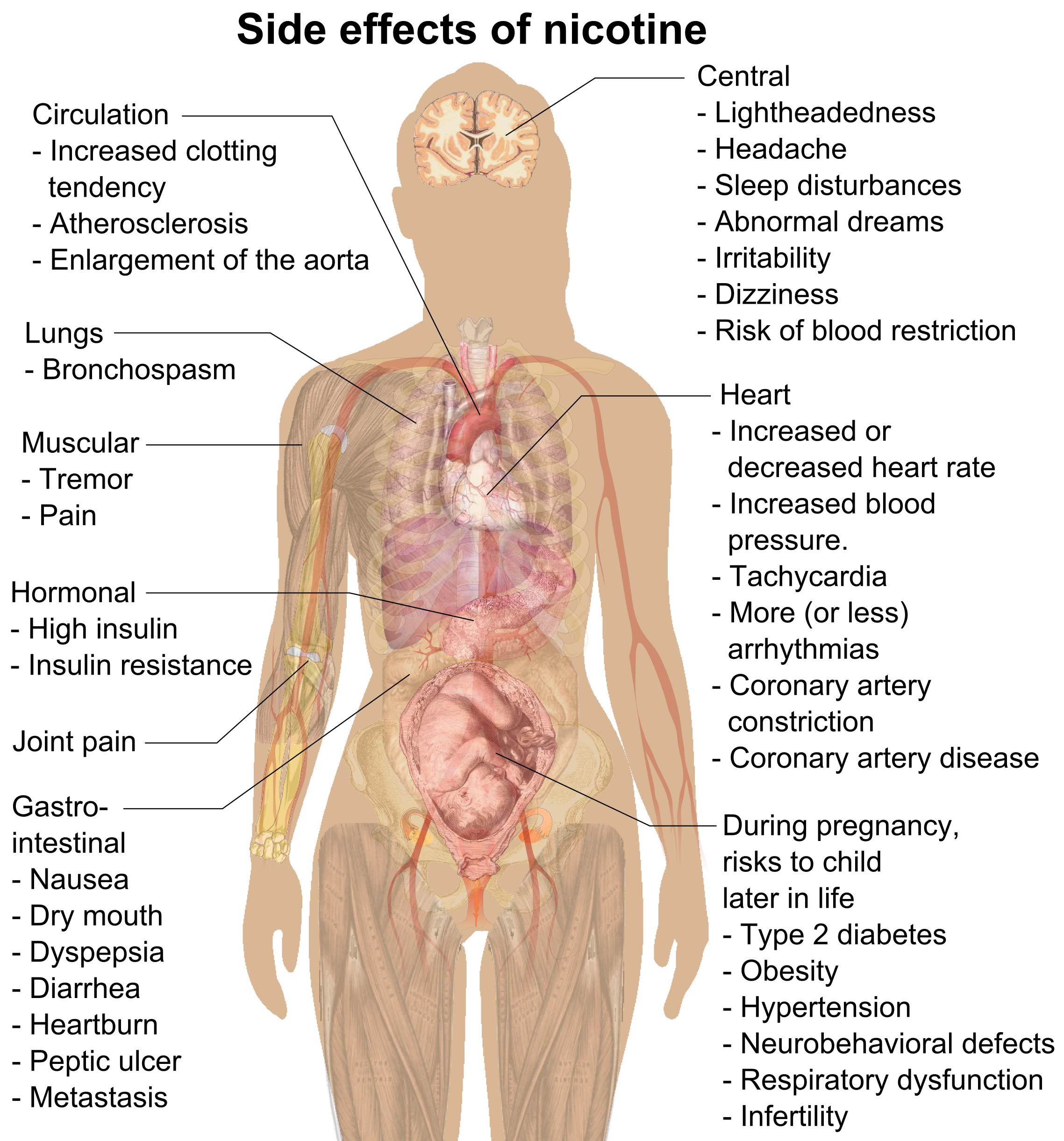
Common side effects depend on the formulation of nicotine.[1] Common side effects with the gum include nausea, hiccups, and irritation of the mouth.[1] Common side effects with the patch include skin irritation and a dry mouth while the inhaler commonly results in a cough, runny nose, or headaches.[1] Serious risks include nicotine poisoning and continued addiction.[1] They do not appear to increase the risk of heart attacks.[8] There are possible harms to the baby if used during pregnancy.[1][11] Nicotine replacement therapy works by reducing cravings caused by nicotine addiction.[1][12]
They were first approved for use in 1984, in the United States.[1] Nicotine replacement products are on the World Health Organization's List of Essential Medicines.[13][14][15] They are available as generic medications.[1]
Medical uses
Nicotine replacement therapy, in the form of gum, patches, nasal spray, inhaler and lozenges all improve the ability of people trying to quit tobacco products.[8] Nicotine replacement therapy is as effective as medications, such as bupropion, in helping people quit smoking for at least six months.[16] All forms of nicotine replacement therapy, including nicotine gum, patches, nasal spray, inhalers, and lozenges, have similar success rates in terms of helping people stop smoking. However, the likelihood that someone will stick to a certain treatment varies, with compliance being the highest with nicotine patches, followed by nicotine gum, inhalers, and nasal sprays.[17] Using a few different nicotine replacement methods in combination may improve success rates in stopping tobacco use.[16][18] Additionally, using nicotine replacement with counseling has been proven to improve tobacco abstinence rates.[19][20] These other strategies include: creating a plan to quit and utilizing quit programs, a quit phone line, or app that provides tips and inspiration to help quit.[18]
Using nicotine replacement therapy to quit smoking should be considered for people who are severely dependent on nicotine.[21] People who are severely dependent include those who smoke: more than one pack per day, within five minutes of awakening, while ill, when they wake up in the middle of the night, to ease withdrawal signs and symptoms.[21]
Nicotine replacement products are most beneficial for heavy smokers who smoke more than 15 cigarettes per day. There are not enough studies to show whether NRT helps those who smoke fewer than 10 cigarettes per day.[20]
Effectiveness
Evaluation of NRT in real-world studies produces more modest outcomes than efficacy studies conducted by industry-funded trials. The National Health Service (NHS) in England has a smoking cessation service based on pharmacotherapy in combination with counseling support. An Action on Smoking and Health (UK) (ASH) report claims that the average cost per life-year gained for every smoker successfully treated by these services is less than £1,000 (below the NICE guidelines of £20,000 per QALY (quality-adjusted life year). However, the investment in NHS stop smoking services is relatively low. A comparison with treatment costs for illicit drug users shows that £585 million is committed for 350,000 problem drug users compared to £56 million for 9 million users of tobacco. This is £6.20 for each smoker, compared to £1,670 per illegal drug user.[22]
The claims for high efficacy and cost-effectiveness of NRT have not been substantiated in real-world effectiveness studies.[23][24][25] Pierce and Gilpin (2002) stated their conclusion as follows: “Since becoming available over the counter, NRT appears no longer effective in increasing long-term successful cessation” (p. 1260).[25] Efficacy studies, which are conducted using randomized controlled trials, do not transfer very well to real-world effectiveness. Bauld, Bell, McCullough, Richardson and Greaves (2009) reviewed 20 studies on the effectiveness of intensive NHS treatments for smoking cessation published between 1990 and 2007.[26] Quit rates showed a dramatic decrease between 4-weeks and one year. A quit rate of 53% at four weeks fell to only 15% at one year. Younger smokers, females, pregnant smokers and more deprived smokers had lower quit rates than other groups.
The efficacy for each of the formulations alone (lozenges, nasal spray, gum, and transdermal patch) to aid in smoking cessation is equal.[27] Efficacy increases 15% to 36% with combining treatments such as gum and lozenges. Higher doses increase the chance of stopping smoking for a period of six months and more. For patches, the most efficient doses were 25 mg worn over 16 hours or 21 mg worn over 24 hours. The evidence suggests that 4 mg nicotine gum leads to higher quit rates compared with 2 mg in heavy smokers.[28]
Toxicity
N-Nitrosonornicotine, a strong carcinogen present in unburned tobacco and cigarette smoke, has been found in the urine of some users of oral NRT products.[29] Nicotine patches is an alternative.
Side effects
Some side effects are caused by the nicotine, and are common to NRT products.[31][32] Other common side effects depend on the formulation of nicotine.[1] Common side effects with the gum include nausea, hiccups, and irritation of the mouth.[1] Common side effects with the patch include skin irritation and a dry mouth while the inhaler commonly results in a cough, runny nose, or headaches.[1] To minimize local skin reactions from the patch, the application site should be moved daily.[33] The nicotine patch can also cause strange dreams if worn while asleep.[20] Nasal sprays commonly cause nasal irritation, watering eyes, and coughing.[31]
Serious risks include nicotine poisoning, which includes symptoms like visual disturbances, hyper-salivation, nausea, and vomiting; and continued addiction to nicotine products.[1] Avoiding smoking and other products with nicotine are recommended since it may lead to nicotine overdose.[34] Although overdose is rare, it can be problematic, especially in children and pets.[35] The symptoms of nicotine overdose include headache, pale skin and mouth, belly pain, weakness, diarrhea, tremors or seizures, agitation, confusion, restlessness, high or low blood pressure, fast or irregular heartbeat, fast breathing, and cold sweats.[21]
Limited evidence exists regarding long-term NRT use.[36]
Safety
Pregnancy
Nicotine is not safe to use in any amount during pregnancy.[37] Nicotine crosses the placenta and is found in the breast milk of mothers who smoke as well as mothers who inhale passive smoke.[38] There are possible harms to the baby if NRT is used during pregnancy.[1][11] Thus, pregnant women and those who are breastfeeding should also consult a physician before initiating NRT.[39] The gum, lozenge, and nasal spray are pregnancy category C. The transdermal patch is pregnancy category D. The transdermal patch is considered less safe for the fetus because it delivers continuous nicotine exposure, as opposed to the gum or lozenge, which delivers intermittent and thus lower nicotine exposure.[40][41]
Strong evidence suggests that nicotine cannot be regarded as a safe substance of cigarette use.[40] Nicotine itself could be at least partly responsible for many of the adverse after birth health results related to cigarette use while the mother was pregnant.[40] There is evidence that nicotine negatively affects fetal brain development and pregnancy outcomes.[42] There is also risk of stillbirth and pre-term birth.[43] Nicotine use will probably harm fetal neurological development.[44] Risks to the child later in life from nicotine exposure during pregnancy include type 2 diabetes, obesity, hypertension, neurobehavioral defects, respiratory dysfunction, and infertility.[32] Nicotine exposure during pregnancy can result in attention deficit hyperactivity disorder (ADHD) and learning disabilities in the child.Template:Fix/category[citation needed] It also puts the child at increased risk for nicotine addiction in the future.[40]
Pregnant women should consider behavioral therapy before NRT is considered.[1]
Youth
In people under the age of eighteen, a physician is often consulted before starting NRT.[39] The evidence suggests that exposure to nicotine between the ages of 10 and 25 years causes lasting harm to the brain and cognitive ability.[45] Evidence is unclear whether adolescents gain benefit from cognitive-behavioral therapy or smoking cessation over the long-term as of 2017.[46] Most tobacco users are under-eighteens when they start, and almost no-one over the age of 25 starts using.[47]
Cardiovascular conditions
While there is no evidence that NRT can increase the risk of heart attacks,[8] individuals with pre-existing cardiovascular conditions or recent heart attacks should consult a physician before initiating NRT.[39]
Smoking is known to cause cardiovascular diseases such as coronary heart disease, hypertension, heart attack, stroke, and peripheral artery disease. Cigarette smoking is the cause of 20% of all cardiovascular deaths in the United States, which is the leading cause of mortality.[48]
Other conditions
Nicotine replacement therapies should be used cautiously in individuals with the following conditions: severe reactive airway diseases (for nasal spray), chronic nasal disorders such as sinusitis, polyps, rhinitis, or allergy (for nasal spray), diabetes (insulin-dependent), gastrointestinal diseases such as esophagitis, active gastric or peptic ulcer disease, liver problems, hyperthyroidism,pheochromocytoma, phenylketonuria (for lozenges), renal problems, and skin conditions such as psoriasis or dermatitis (for the transdermal patch).[49]
Mechanism of action
Nicotine replacement therapy works by reducing cravings due to nicotine addiction.[1][12] Smoking cigarettes releases high doses of nicotine to the brain in a matter of seconds as opposed to low doses released over a period of minutes to hours by the various forms of nicotine replacement therapy.[33] Nicotine from NRT does not reach as high a concentration in the blood as does nicotine from smoke inhalation due to different absorption methods. NRT relies on systemic venous absorption, whereas nicotine from cigarettes reaches the arterial system.[33] Nicotine replacement products vary in the time it takes for the nicotine to enter the body and the total time nicotine stays in the body.[19] The more quickly a dose of nicotine is delivered and absorbed, the higher the addiction risk.[50] It is possible to become dependent on some NRTs.[51]
Nicotine patches are applied to the skin and continuously administer a stable dose of nicotine slowly over 16–24 hours.[19][41] Nicotine gum, nicotine sprays, nicotine toothpicks, nicotine sublingual tablets, and nicotine lozenges administer nicotine orally with quicker nicotine uptake into the body but lasting a shorter amount of time.[52] Nicotine inhalers are metered-dose inhalers Template:Fix/category[citation needed] that administer nicotine through the lungs and mucous membranes of the throat quickly, lasting for a short amount of time. For example, blood nicotine levels are the highest 5–10 minutes after using the nicotine nasal spray, 20 minutes after using a nicotine inhaler or chewing nicotine gum, and 2–4 hours after using a nicotine patch.[19][53]
Society and culture
NRT products were first approved for use in the United States in 1984.[1] Nicotine replacement products are on the World Health Organization's List of Essential Medicines..[13] They are available as generic medication.[1]
Formulations
| NRT Type | Device/package | Availability | How it works[54][55] |
|---|---|---|---|
| Patch | Pouch | Over-the-counter | 16 or 24 hours sustained-release transdermal patch |
| Lozenge | Blister pack | Over-the-counter | 20 to 30 minutes modified-release dosage tablet containing nicotine polacrilex |
| Sublingual tablets | Blister pack | Over-the-counter | Quickly dissolves to releases nicotine through a hard candy |
| Gum | Blister pack | Over-the-counter | Chewing the gum releases nicotine as a modified-release dosage |
| Mouth spray | Mouth spray bottle | Over-the-counter | Spraying a mist into the mouth administers nicotine for buccal administration |
| Vapour inhalator | Nicorette Inhalator: with 10 mg nicotine disposable cartridges | Over-the-counter | Resembles cigarettes; A disposable cartridge contains about 10 mg nicotine (about 40% is released). Multiple inhaling through the mouthpiece administers sufficient nicotine. |
| Pressurized Metered-dose inhaler (pMDI) | Prescription | Inhaling through the mouthpiece administers nicotine | |
| Nasal spray | Nasal spray bottle | Prescription | Spraying a pump bottle into the nose administers nicotine |
The nicotine patch is a once-daily, longer-acting form of NRT. An advantage of the nicotine patch is its simple compliance; it does not require active use throughout the day.[33] The gum, lozenge, sublingual tablet, oral inhaler, oral spray, and nasal spray are acutely dosed products, providing the user with the benefit and ability of self-titrating based on cravings.[33]
Brand names include Commit Lozenge, Nicoderm, Nicogum, Nicorette, Nicotex, Nicotinell, and Thrive. NRT products contain similar pharmaceutical grade nicotine as is used in e-cigarettes.Template:Fix/category[citation needed]
Medicines
In 2015, the United States Public Health Service listed seven agents for the stopping of tobacco, which included five nicotine replacement treatments (nicotine patches, gum, lozenges, inhalers, and nasal sprays) and two oral medications (bupropion and varenicline). Other NRT options are available, including nicotine mouth sprays and sublingual tablets.[56]
Dosing
The dose of nicotine replacement therapy products is generally based on if the user is considered a heavy, average, or light smoker.[21]
| Type of User | Dose of NRT | Amount of cigarettes | Amount of smokeless tobacco |
|---|---|---|---|
| Light | Lower | <10 cigarettes daily | <2 snuff cans or tobacco pouches weekly |
| Average | Moderate | 10-20 cigarettes daily | 2-3 snuff cans or tobacco pouches weekly |
| Heavy | Higher | 1 or more pack of cigarettes daily | >3 snuff cans or tobacco pouches weekly |
A cigarette delivers an average of 1 mg to 3 mg of the nicotine contained in it. NRT products typically aim to parallel this, but the amount of nicotine absorbed by the user is less than the original dose.
Nicotine nasal sprays are formulated in doses of lowest strength, available in 0.5 mg and 1 mg strengths.
Nicotine lozenges deliver doses as low as 1 mg up to 4 mg. It is not chewed as the gum would be, and dissolves in approximately 30 minutes.[33] This formulation may be preferred by those individuals who do not find gum chewing to be acceptable.
Nicotine gum is available in doses of 2 mg and 4 mg. Using 4 mg nicotine gum versus 2 mg gum increases the likelihood of successful smoking cessation.[28] When using the gum, acidic beverages like soda, coffee, or beer should be avoided fifteen minutes prior and during use because they can impede proper absorption of nicotine.[33]
Nicotine inhalers come in 10 mg and 15 mg cartridge strengths and typically deliver around 4 mg in one dose.[57] The inhaler may be preferred in individuals who want to satisfy the hand-to-mouth ritual that smoking provides.[33]
Transdermal patches deliver between 5 mg and 52.5 mg of nicotine, which results in plasma levels similar to that of heavy smokers. Combining nicotine patch treatment with a faster nicotine-delivery means, like nicotine gum or spray, improves the likelihood of successful treatment.[28][8]
Not approved as NRTs
Some smokeless consumer products available can function as alternative nicotine delivery systems (ANDS)[58] but they have not received FDA approval as smoking-cessation therapy aids that are safe and effective.
Snus and nasal snuff also allow for nicotine administration outside of tobacco smoking.[59] Nicotine pouches are described as similar to or a tobacco-free variant of snus. They are pre-portioned and are held in the user's lip or cheek allowing for sublingual or buccal delivery of flavors and high doses of nicotine. The small pouches are not like chewing tobacco, as the user does not need to spit since the contents of the pouches stay inside during use. Swedish pouches have been available on the American consumer market since at least 2016[60] but their popularity and controversy surged in 2019 & 2020. In the US and UK concerns have been raised that nicotine pouches are seemingly too similar to banned snus products, is aimed at teenagers, further complicating the youth vaping trend,[61] falling into the hands of adolescents easily, and are discrete enough to easily pass for regular gums or lozenges.[62][63]
Nicotine infused toothpicks are another product that has been available in the United States since at least 2013. They can have a total nicotine delivery that is comparable to that of nicotine gum.[52] Nicotine toothpicks generally are infused with food-grade flavorings and 1–3 mg of nicotine, which is similar to that of other oral-delivery nicotine products and some cigarettes.[64] In spite of these similarities, as of 2018 they have been a subject of controversy. Online retailers have been under scrutiny for allowing their products to be too easily purchased by youth.[65][66][67] Various news outlets and school districts have expressed the concern that these products have a high appeal to minors wanting to experiment with nicotine due to; the multitude of sweet flavors offered, ease & speed of use, seeming innocuous, and having a discrete nature.[68][69][70] In 2015, NRT sales fell for the first time since 2008 while sales for e-cigarettes or electronic nicotine delivery systems (ENDS) continued to increase at a substantial rate. The evidence is that UK smokers are trying to quit with e-cigarettes rather than NRT methods.[71]
E-cigarettes are often, although not always, designed to look and feel like cigarettes. They have been marketed as less harmful alternatives to cigarettes,[72] but very few are as yet approved as NRTs in any jurisdiction. Some electronic cigarettes have coarsely adjustable nicotine levels. Some healthcare groups have hesitated to recommend e-cigarettes for quitting smoking, because of limited evidence of effectiveness and safety.[73] However, more recent review show the opposite, possibly because of newer types of e‐cigarettes have better nicotine delivery than older one.[74]
The U.S. Food and Drug Administration (FDA) has a list of additional tobacco products they are seeking to regulate, including electronic cigarettes.[75] Most approved NRT products have been approved for over 20 years,[76] however the FDA has also approved nicotine inhalers as a form of NRT.[77][78]
Future approaches of NRT could include nicotine preloading, a true pulmonary inhaler, and nicotine vaccines.[8] Nicotine preloading, otherwise known as pre-cessation or pre-quitting NRT, has found that using the patch for a few weeks before the quit date produces significantly higher quit rates than if it was started on the quit day.[8] The true pulmonary inhaler would deliver nicotine to the lungs in a manner that more resembles cigarette smoking, which would provide better relief of background cravings as well as acute cravings.[8] Nicotine vaccines are under investigation as a method to treat tobacco dependence through priming the body to mount an immune response against nicotine.[8]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 "Nicotine". The American Society of Health-System Pharmacists. Archived from the original on 18 December 2015.
- ↑ "Nicoderm CQ- nicotine patch, extended release". DailyMed. Retrieved 26 January 2022.
- ↑ "Commit - nicotine lozenge". DailyMed. Retrieved 26 January 2022.
- ↑ "Nicorette- nicotine polacrilex lozenge". DailyMed. Retrieved 26 January 2022.
- ↑ "Nicorette White Ice Mint- nicotine polacrilex gum, chewing Nicorette Original- nicotine polacrilex gum, chewing Nicorette Cinnamon Surge- nicotine polacrilex gum, chewing Nicorette Fresh Mint- nicotine polacrilex gum, chewing Nicorette Mint- nicotine polacrilex gum, chewing Nicorette Spearmint Burst- nicotine polacrilex gum, chewing". DailyMed. Retrieved 26 January 2022.
- ↑ Jain R, Majumder P, Gupta T (2013). "Pharmacological intervention of nicotine dependence". BioMed Research International. 2013: 278392. doi:10.1155/2013/278392. PMC 3891736. PMID 24490153.
- ↑ Smith KD, Scott MA, Ketterman E, Smith PO (April 2005). "Clinical inquiries. What interventions can help patients stop using chewing tobacco?". The Journal of Family Practice. 54 (4): 368–9. PMID 15833231.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 Hartmann-Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T (May 2018). Cochrane Tobacco Addiction Group (ed.). "Nicotine replacement therapy versus control for smoking cessation". The Cochrane Database of Systematic Reviews. 5 (5): CD000146. doi:10.1002/14651858.CD000146.pub5. PMC 6353172. PMID 29852054.
- ↑ McDonough M (August 2015). "Update on medicines for smoking cessation". Australian Prescriber. 38 (4): 106–11. doi:10.18773/austprescr.2015.038. PMC 4653977. PMID 26648633.
Evidence suggests that combinations of nicotine replacement therapy may be more effective than using a single formulation
- ↑ Cahill K, Stevens S, Perera R, Lancaster T (May 2013). "Pharmacological interventions for smoking cessation: an overview and network meta-analysis". The Cochrane Database of Systematic Reviews. 5 (5): CD009329. doi:10.1002/14651858.CD009329.pub2. PMC 8406789. PMID 23728690. S2CID 205199430.
Combination NRT also outperformed single formulations
- ↑ 11.0 11.1 De Long NE, Barra NG, Hardy DB, Holloway AC (December 2014). "Is it safe to use smoking cessation therapeutics during pregnancy?". Expert Opinion on Drug Safety. 13 (12): 1721–31. doi:10.1517/14740338.2014.973846. PMID 25330815. S2CID 207488115.
- ↑ 12.0 12.1 Nicotine Replacement Therapy for Smoking Cessation or Reduction: A Review of the Clinical Evidence (Report). Canadian Agency for Drugs and Technologies in Health. 16 January 2014. PMID 24741730.
- ↑ 13.0 13.1 World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ↑ World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- ↑ "Nicotine Replacement Therapy (NRT) (Inclusion)". World Health Organization. 11 December 2010. Archived from the original on February 13, 2010. Retrieved 28 May 2020.
- ↑ 16.0 16.1 Cahill K, Stevens S, Perera R, Lancaster T (May 2013). "Pharmacological interventions for smoking cessation: an overview and network meta-analysis". The Cochrane Database of Systematic Reviews. 5 (5): CD009329. doi:10.1002/14651858.CD009329.pub2. PMC 8406789. PMID 23728690. S2CID 205199430.
- ↑ Hajek P, West R, Foulds J, Nilsson F, Burrows S, Meadow A (September 1999). "Randomized comparative trial of nicotine polacrilex, a transdermal patch, nasal spray, and an inhaler". Archives of Internal Medicine. 159 (17): 2033–8. doi:10.1001/archinte.159.17.2033. PMID 10510989.
- ↑ 18.0 18.1 "Using Nicotine Replacement Therapy | Smokefree". smokefree.gov. Retrieved 2019-10-23.
- ↑ 19.0 19.1 19.2 19.3 Rigotti NA (February 2002). "Clinical practice. Treatment of tobacco use and dependence". The New England Journal of Medicine. 346 (7): 506–12. doi:10.1056/nejmcp012279. PMID 11844853.
- ↑ 20.0 20.1 20.2 "Nicotine replacement therapy". MedlinePlus. U.S. National Library of Medicine. Archived from the original on 9 January 2015. Retrieved 28 October 2014.
- ↑ 21.0 21.1 21.2 21.3 21.4 "Nicotine Replacement Therapy for Quitting Tobacco". www.cancer.org. Retrieved 2019-10-28.
- ↑ "Action on Smoking & Health, 2008" (PDF). Archived from the original (PDF) on 24 September 2015. Retrieved 27 August 2015.
- ↑ Doran CM, Valenti L, Robinson M, Britt H, Mattick RP (May 2006). "Smoking status of Australian general practice patients and their attempts to quit". Addictive Behaviors. 31 (5): 758–66. doi:10.1016/j.addbeh.2005.05.054. PMID 16137834.
- ↑ Bauld L, Boyd KA, Briggs AH, Chesterman J, Ferguson J, Judge K, Hiscock R (February 2011). "One-year outcomes and a cost-effectiveness analysis for smokers accessing group-based and pharmacy-led cessation services". Nicotine & Tobacco Research. 13 (2): 135–45. doi:10.1093/ntr/ntq222. PMID 21196451.
- ↑ 25.0 25.1 Pierce JP, Gilpin EA (September 2002). "Impact of over-the-counter sales on effectiveness of pharmaceutical aids for smoking cessation". JAMA. 288 (10): 1260–4. doi:10.1001/jama.288.10.1260. PMID 12215133.
- ↑ Bauld L, Bell K, McCullough L, Richardson L, Greaves L (March 2010). "The effectiveness of NHS smoking cessation services: a systematic review". Journal of Public Health. 32 (1): 71–82. doi:10.1093/pubmed/fdp074. PMID 19638397.
- ↑ Abuse, National Institute on Drug. "What are treatments for tobacco dependence?". www.drugabuse.gov. Retrieved 2019-11-20.
- ↑ 28.0 28.1 28.2 Lindson N, Chepkin SC, Ye W, Fanshawe TR, Bullen C, Hartmann-Boyce J (April 2019). "Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation". The Cochrane Database of Systematic Reviews. 2019 (4): CD013308. doi:10.1002/14651858.CD013308. PMC 6470854. PMID 30997928.
- ↑ Stepanov, I; Carmella, SG; Briggs, A; Hertsgaard, L; Lindgren, B; Hatsukami, D; Hecht, SS (1 November 2009). "Presence of the carcinogen N'-nitrosonornicotine in the urine of some users of oral nicotine replacement therapy products". Cancer Research. 69 (21): 8236–40. doi:10.1158/0008-5472.CAN-09-1084. PMC 2783463. PMID 19843845.
- ↑ Detailed reference list is located on a separate image page
- ↑ 31.0 31.1 "Nicotine Side Effects". Drugs.com. Drugs.com. 21 January 2019.
- ↑ 32.0 32.1 Schraufnagel DE, Blasi F, Drummond MB, Lam DC, Latif E, Rosen MJ, et al. (September 2014). "Electronic cigarettes. A position statement of the forum of international respiratory societies". American Journal of Respiratory and Critical Care Medicine. 190 (6): 611–8. doi:10.1164/rccm.201407-1198PP. PMID 25006874. S2CID 43763340.
- ↑ 33.0 33.1 33.2 33.3 33.4 33.5 33.6 33.7 Wadgave U, Nagesh L (July 2016). "Nicotine Replacement Therapy: An Overview". International Journal of Health Sciences. 10 (3): 425–35. doi:10.12816/0048737. PMC 5003586. PMID 27610066.
- ↑ "Nicotine Replacement Therapy for Quitting Tobacco". www.cancer.org. Retrieved 20 November 2019.
- ↑ "Nicotine Replacement Therapy for Quitting Tobacco".
- ↑ Wilder N, Daley C, Sugarman J, Partridge J (April 2016). "Nicotine without smoke: Tobacco harm reduction". UK: Royal College of Physicians. p. 58. Archived from the original on 2016-05-05.
- ↑ Alawsi F, Nour R, Prabhu S (August 2015). "Are e-cigarettes a gateway to smoking or a pathway to quitting?". British Dental Journal. 219 (3): 111–5. doi:10.1038/sj.bdj.2015.591. PMID 26271862. S2CID 24120636.
- ↑ "State Health Officer's Report on E-Cigarettes: A Community Health Threat" (PDF). California Department of Public Health. January 2015.
- ↑ 39.0 39.1 39.2 "FDA 101: Smoking Cessation Products". U.S. Food and Drug Administration. Archived from the original on 3 November 2014. Retrieved 28 October 2014.
- ↑ 40.0 40.1 40.2 40.3 Bruin JE, Gerstein HC, Holloway AC (August 2010). "Long-term consequences of fetal and neonatal nicotine exposure: a critical review". Toxicological Sciences. 116 (2): 364–74. doi:10.1093/toxsci/kfq103. PMC 2905398. PMID 20363831.
- ↑ 41.0 41.1 Oncken C, Dornelas E, Greene J, Sankey H, Glasmann A, Feinn R, Kranzler HR (October 2008). "Nicotine gum for pregnant smokers: a randomized controlled trial". Obstetrics and Gynecology. 112 (4): 859–67. doi:10.1097/AOG.0b013e318187e1ec. PMC 2630492. PMID 18827129.
- ↑ Lushniak BD, Samet JM, Pechacek TF, Norman LA, Taylor PA (2014). "Chapter 5 – Nicotine". The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Surgeon General of the United States, National Center for Chronic Disease Prevention Health Promotion (US) Office on Smoking Health. pp. 107–138. PMID 24455788.
- ↑ Lushniak BD, Samet JM, Pechacek TF, Norman LA, Taylor PA (2014). "Chapter 9 – Reproductive Outcomes". The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General (PDF). Surgeon General of the United States. pp. 107–138. PMID 24455788.
- ↑ England LJ, Kim SY, Tomar SL, Ray CS, Gupta PC, Eissenberg T, et al. (31 December 2010). "Non-cigarette tobacco use among women and adverse pregnancy outcomes". Acta Obstetricia et Gynecologica Scandinavica. 89 (4): 454–64. doi:10.3109/00016341003605719. PMC 5881107. PMID 20225987.
The use of any products containing nicotine likely will have adverse effects of fetal neurological development.
- ↑ E-Cigarette Use Among Youth and Young Adults (PDF). A Report of the Surgeon General (Report). Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. 2016. Retrieved 15 November 2018.
Evidence for this report was gathered from scientific research that included one or more of three age groups. These age groups included young adolescents (11–13 years of age), adolescents (14–17 years of age), and young adults (18–24 years of age). Some studies refer to the younger groups more generally as youth... Of concern with regard to current trends in e-cigarette use among youth and young adults, the evidence suggests that exposure to nicotine during this period of life may have lasting deleterious consequences for brain development, including detrimental effects on cognition
- ↑ Fanshawe TR, Halliwell W, Lindson N, Aveyard P, Livingstone-Banks J, Hartmann-Boyce J (November 2017). "Tobacco cessation interventions for young people". The Cochrane Database of Systematic Reviews. 2017 (11): CD003289. doi:10.1002/14651858.cd003289.pub6. PMC 6486118. PMID 29148565.
- ↑ E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General (Report). Rockville, MD: U.S. Department of Health and Human Services, Public Health Service Office of the Surgeon General. 2016. Retrieved 15 November 2018.
The majority of tobacco users start before they are 18 years of age, and almost no one starts after age 25
- ↑ "How Smoking Affects Heart Health". FDA. FDA. 2019-04-18. Retrieved 6 November 2019.
- ↑ "Nicotine Monograph for Professionals". Drugs.com. Retrieved 20 November 2019.
- ↑ Parrott AC (July 2015). "Why all stimulant drugs are damaging to recreational users: an empirical overview and psychobiological explanation" (PDF). Human Psychopharmacology. 30 (4): 213–24. doi:10.1002/hup.2468. PMID 26216554. S2CID 7408200.
- ↑ Hughes JR (1989). "Dependence potential and abuse liability of nicotine replacement therapies". Biomedicine & Pharmacotherapy. 43 (1): 11–7. doi:10.1016/0753-3322(89)90185-6. PMID 2659095.
- ↑ 52.0 52.1 Hasenfratz M, Bättig K (October 1991). "Nicotine absorption and the subjective and physiologic effects of nicotine toothpicks". Clinical Pharmacology and Therapeutics. 50 (4): 456–61. doi:10.1038/clpt.1991.164. PMID 1914382. S2CID 23299185.
- ↑ Package insert monograph with Nicorette inhaler
- ↑ CDCTobaccoFree (2019-06-04). "Learn About Nicotine Replacement Therapy". Centers for Disease Control and Prevention. Retrieved 2019-10-28.
- ↑ Nonprescription Drugs Advisory Committee (September 18, 2019). "Nicotine Mouth Spray, 1 mg" (PDF). www.fda.gov.
- ↑ Fiore MC, Jaen CR, Baker TB, et al. "Treating tobacco use and dependence: 2008 update" (PDF). US Department of Health and Human Services. Archived from the original (PDF) on 2015-08-23. Retrieved 2015-08-28.
- ↑ "pharmacologic product guide: FDA-Approved Medications for Smoking Cessation" (PDF). American Academy of Family Physicians. 17 January 2019. Retrieved 29 July 2019.
- ↑ Pearson, Jennifer L.; Smiley, Sabrina L.; Rubin, Leslie F.; Anesetti-Rothermel, Andrew; Elmasry, Hoda; Davis, Megan; DeAtley, Teresa; Harvey, Emily; Kirchner, Thomas; Abrams, David B. (1 April 2016). "The Moment Study: protocol for a mixed method observational cohort study of the Alternative Nicotine Delivery Systems (ANDS) initiation process among adult cigarette smokers". BMJ Open. 6 (4): e011717. doi:10.1136/bmjopen-2016-011717. ISSN 2044-6055. PMC 4854005. PMID 27105716.
- ↑ Phillips CV, Heavner KK (July 2009). "Smokeless tobacco: the epidemiology and politics of harm". Biomarkers. 14 (Suppl 1): 79–84. doi:10.1080/13547500902965476. PMID 19604065. S2CID 9883931.
- ↑ "Nicotine pouches fast-growing sub category".
- ↑ "Concern over nicotine pouches targeting teens". WKBW Buffalo. October 16, 2019.
- ↑ "Nicotine pouch craze swiping fifes playgrounds". thecourier.
- ↑ "Warning over children using nicotine pouches". 11 December 2020.
- ↑ "Adjusting to Changing Tobacco Trends". Convenience Store News. Retrieved 2019-07-30.
- ↑ "Officials warn of nicotine toothpick use by teens". timesfreepress.com. 2019-01-13. Retrieved 2019-07-30.
- ↑ "Students are getting their hands on nicotine toothpicks". Wtol11.
- ↑ "In the Wake of Heightened Regulatory Scrutiny of Vaping Products, Nicotine-Containing Toothpicks are Next to Come Under Fire by FDA". The National Law Review. Retrieved 2020-11-12.
- ↑ Spence R (2018-03-26). "Nicotine toothpicks causing problems some mid-Michigan schools". WEYI. Retrieved 2019-07-30.
- ↑ "Nicotine-Infused Toothpicks Showing Up in Smoke Shops". NBC 5 Dallas-Fort Worth. Retrieved 2019-07-30.
- ↑ Morgan T (2019-02-25). "Schools looking out for nicotine-infused toothpicks as they also combat vaping among teens". WSYX. Retrieved 2019-07-30.
- ↑ "STS Documents - Smoking In England". www.smokinginengland.info. Retrieved 2021-01-31.
- ↑ "Electronic cigarettes (also known as vapourisers)" (PDF). Action on Smoking and Health. Archived from the original (PDF) on 21 November 2015. Retrieved 10 November 2014.
- ↑ McRobbie H, Bullen C, Hartmann-Boyce J, Hajek P (2014). McRobbie H (ed.). "Electronic cigarettes for smoking cessation and reduction". The Cochrane Database of Systematic Reviews. 12 (12): CD010216. doi:10.1002/14651858.CD010216.pub2. PMID 25515689. S2CID 205203797.
- ↑ Hartmann-Boyce, J; McRobbie, H; Butler, AR; Lindson, N; Bullen, C; Begh, R; Theodoulou, A; Notley, C; Rigotti, NA; Turner, T; Fanshawe, TR; Hajek, P (14 September 2021). "Electronic cigarettes for smoking cessation". The Cochrane database of systematic reviews. 9 (9): CD010216. doi:10.1002/14651858.CD010216.pub6. PMID 34519354.
- ↑ "Electronic Cigarettes (e-Cigarettes)". U.S. Food and Drug Administration. Archived from the original on 2014-11-17. Retrieved 2014-11-06.
- ↑ Office of the Commissioner (2018-11-14). "4 Tips to Quit Smoking". FDA.
- ↑ Drummond MB, Upson D (February 2014). "Electronic cigarettes. Potential harms and benefits". Annals of the American Thoracic Society. 11 (2): 236–42. doi:10.1513/annalsats.201311-391fr. PMC 5469426. PMID 24575993.
- ↑ DeNoon DJ. "New Nicotine Inhaler May Help Smokers Quit". WebMD. Retrieved 2019-07-30.
External links
- "Nicotine". Drug Information Portal. U.S. National Library of Medicine.
- University of Wisconsin Center for Tobacco Research and Intervention
- Recommendations for special populations
- "Nicotine Lozenges". MedlinePlus. 2018-08-15.
- "Nicotine Nasal Spray". MedlinePlus. 2016-07-15.
- "Nicotine Oral Inhalation". MedlinePlus. 2016-07-15.
- "Nicotine Gum". MedlinePlus. 2017-10-15.
Script error: No such module "Portal bar".
- Articles with short description
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Articles without EBI source
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without InChI source
- Articles containing unverified chemical infoboxes
- Commons category link is defined as the pagename
- Smoking cessation
- Substance-related disorders
- GSK plc brands
- World Health Organization essential medicines
- Wikipedia medicine articles ready to translate